Brief
Anatomy
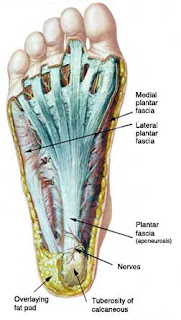
The
plantar fascia is a thick band of connective tissue with investing layers from
the calcaneal (heel) tuberosity to the base of the metatarsals, creating a
mobile yet stable soft tissue foundation for the medial and transverse arches
of the foot.
The
plantar fascia is composed of type 1 collagen
(a thick protein arranged in parallel bundles) with the ability to
resist high loads of tensile stress. It is considered a non-contractile tissue
responding to the mechanical loads placed upon it. It has poor ability to
stretch much beyond 4% of its resting length. The plantar fascia is prone to
degenerative changes in response to chronic overuse and increasing with age
related changes in the connective tissues.
There are
3 nerves that travel through the various layers of the plantar fascia from the
medial (inside) portion of the ankle. The medial calcaneal nerve, the lateral
plantar nerve and the medial plantar nerve all arise from the larger tibial
nerve. These often play a role in plantar fascia pain with the medial calcaneal
nerve often commonly involved as it wraps around the tuberosity.
Function
The
plantar fascia maintains the longitudinal and transverse arches of the foot and
also serves to dampen pronation. As the foot contacts the ground and continues
through to mid stance the plantar fascia lengthens under load almost causing a
breaking effect, thus absorbing load. This sets the stage for the foot to then
supinate creating a more rigid structure for toe off.
If the
plantar fascia undergoes degenerative changes (collagen disarray, neovessel in
growth, fibrosis etc) the structure become less mobile and less resistant to
tensile load. This creates further overload on already compromised structure.
Onset
Plantar
fascia pain usually appears with a gradual onset. Initially there is stiffness
(and pain) on arising only to warm up 5 minutes later. The pain gradually
progresses to pain on warm up and sometimes warm down. There is often a period
of weeks to months where the patient does not seem to regress. Often
this is where the running athlete does not present for treatment thinking “it’s
not getting worse!”. Despite no notable regression the connective tissue may
still degenerate under repetitive loads.
Over time
if the athlete continues to run there will be a point where pain is constant
through out the run. This is usually the first time a clinician will see the
runner often months into the process.
Causes
The
causes are likely multifactorial:
- Increase in volume
- Increase in intensity
- Change in training surface
- Change in footwear (or lack of)
- Reduced dorsiflexion
- Excessive pronation
- Reduced great toe extension
Pronation – a possible causative factor
Prognosis
The
prognosis for plantar fascia pain is less reliable than for a straight - forward
muscle tear. The quicker the injury is addressed the better the outcome.
Plantar fascia pain is similar to a tendinopathy in nature, with degeneration
of the connective tissue a classical finding under ultrasound. Depending on the
location within the plantar fascia, will depend on the type of tissue you are
dealing with. For example, a degenerative enthesopathy (insertion onto the
tuberosity of the heel) will involve various connective tissues, possibly fat
pad and underlying soft tissues. If the focus is in the body of the plantar
fascia it may be a case of the connective tissue composition (type 1 collagen).
If
addressed early, clinical evidence would suggest you may be looking at 6-12
weeks recovery.
Chronic
ongoing plantar heel pain injuries can be as long as 6 months to 2 years with
high re-occurrence rates.
“The Doc
says I have heel spurs!”
A basic
understanding of the anatomy helps to understand the pathogenesis. As stated, the
plantar fascia attaches to the calcaneal (heel) tuberosity. In some cases
abnormal mechanics may place an increased demand upon the attachment leading to
an increase in bone loading, hence, size of the tuberosity.
There is
no evidence to suggest that an increase in bone (the so-called heel spurs) is a
causative factor in pain. In fact some asymptomatic patients (no symptoms) have
enlarged calcaneal tuberosities. It is therefore important to look to the
causative factors and ways of managing plantar fascia heel pain. A ‘spur’ is
not a sign of plantar fascia pain. The painful site is usually close to the
attachment and may be involved in some cases.
Treatment
Plantar
fascia pain presents in a similar fashion to a tendinopathy and as such should
be treated as one. There is little evidence to suggest inflammation to be a
factor in plantar fascia heel pain. In this case the treatment protocol will be
lengthy. Addressing the causative factor(s) is paramount.
Treatment options include:
Soft
tissue therapy to focal areas of thickening especially in the posterior lower
limb if reduced dorsiflexion is a factor. Joint mobilisation and local stretching may
improve the outcome. Clinically local soft tissue work to mobilise thickened areas
within the plantar fascia may be warranted.
Controlling
excessive pronation with strengthening of tibialis posterior (inside of calf)
and gluteus medius (lateral hip) or with the use of orthoses. Biomechanics
during the gait cycle may have an important role to play. Overall reducing load
on the plantar fascia. Low dye taping may help in the short term as a means of
gaining proprioception and further reducing load
Further
soft tissue treatment may help with overloaded structures (areas of increased tone)
that alter gait as a compensatory mechanism or as a cause of the injury itself.
Address
footwear* (or lack of – think barefoot running) - this is a hot topic at the
moment! Whichever way you decide to go, make it a slow transition and be sure
to use progressive over load and recovery techniques in your training program.
Consider
consequences further up the chain eg; reduced torso rotation can create
compensation through increase rotation of the femur, tibia and pronation. The
net effect is loading of the plantar fascia. Consider the whole kinetic chain.
Low dye taping may help
What about rolling on a golf ball?
This may
work to minimise the symptoms temporarily, however it will do little to help
with the driving factors. Very rarely do we find in clinical practice the
plantar fascia to be tight. It is important to consider the anatomy and
function when considering the goal of any treatment. The plantar fascia is a
thick piece of connective tissue with very little stretch – do we really need
to try and stretch it?
Is it always plantar fascia involvement?
This
discussion has focused on pain in the plantar fascia. There are numerous causes
of pain in the plantar surface of the foot,
the location will be a key to further possibilities such as:
- Fat pad contusion (heel)
- Plantar fascia tear (grade?)
- Sesamoiditis
- Morton’s neuroma
- Stress fracture of the cuboid
- Stress fracture of the calcaneus
- Medial calcaneal nerve compression (common)
Summary
Plantar
fascia pain is common in runners and often lengthy to treat. By the time the
running athlete has presented to healthcare professionals there is usually a
long history. Plantar fascia pain is degenerative in nature thus occurring over
time. An earlier treatment program will likely give a better prognosis.
· If you
would like to read some great articles on the science for and against bare foot
running go to the science of sport website www.sportsscientists.com
For those
interested in further reading Clinical Sports Medicine, Brukner and Khan, 2007,
have some excellent information and practical tips
For now,
Jimmy


No comments:
Post a Comment